The Essential Vaccines You Must Give to Your Dog
There is no need to emphasize the substantial benefits of vaccination.
It is the best way to fight against infectious diseases, and to prevent the outbreak of epidemics.
As some of these infections can be transmitted to humans, vaccinating dogs is also a matter of public health.
Moreover, the rabies vaccine is mandatory in numerous regions of the world.
But, it does not mean we should “over-vaccinate” our dogs.
Because there are still some risks associated with the administration of vaccines even though they are rare: attenuated vaccines can revert and become virulent again. Erythema, spots, allergic reactions or infections at the injection site are also possible.
The other issue is that vaccines come at a cost. Either the money would be better spent than on a vaccine which is not absolutely necessary. Or an excessive cost could dissuade some dog owners to do any kind of vaccination or give the necessary boosters.
The issue here is to select the vaccines your dog really needs:
But, how should they be selected?
Fortunately, a board of international veterinary experts (the Vaccination Guidelines Group) of the World Small Animal Veterinary Association issued recommendations on pets vaccination to help vet practitioners design vaccination programs.
These recommendations are acknowledged and adapted by other groups of experts at a National level such as the AAHA (American Animal Hospital Association) in the US or the VMD (Veterinary Medicine Directorates) in the UK.
The experts distinguish:
- The vaccines recommended for all dogs whatever the circumstances. They are the core vaccines
- The non-core vaccines are optional. Their use depends on your dog's risk factors.
VGG’s statement:
We should aim to vaccinate every animal with core vaccines.
Non-core vaccines should be given no more frequently than is deemed necessary.
In its analysis, the VGG decided to focus on vaccines against viruses that:
- cause serious and often fatal diseases
- are contagious enough to spread rapidly across the dog population
- can be controlled efficiently by available vaccines
- are not subject to important regional variation (i.e. potentially exist worldwide)
Core vaccines protect dogs against:
- Rabies
- Canine Distemper Virus
- Canine Adenovirus types 1 & 2
- Canine Parvovirus type 2
Vaccination schedule for core vaccines
Core vaccines are all live attenuated vaccines that induce a strong response from the immune system both humoral and cell-mediated.
Adenovirus, parvovirus and distemper virus vaccines
Young puppies should be vaccinated 3 times, from 4-6 weeks of age, 2-3 weeks apart.
A booster will be administered at 6 months or 1 year of age, and then every 3 years.
Rabies
The first injection takes place at 12 weeks and sometimes a booster may be injected 4 weeks later.
Adult dogs receive a booster either every year or every 3 years according to the manufacturer recommendations and to the regional regulation.

Rabies
Rabies holds a special place among pet infectious diseases, because it can be transmitted from dogs, or wild species, to humans. And always turns out to be fatal for both humans and animals, if left untreated.
Vaccination against rabies also represents a key step in the vaccination history. It is the first vaccine ever designed, after Dr Jenner’s discovery of the variolation principle (see Chapter 2).
Because rabies is a threat to Public Health, Health Authorities’ policies aim at eradicating the virus, which is almost done in many developed countries.
Vaccination against rabies is more than a recommendation. It is a legal requirement in many states in the US.
In the European Union, whenever you need to travel abroad with your pet you’ll need to prove that it is properly vaccinated against rabies, either by a certificate, a microchip or a blood/serum test.
You should know what the regulation in your region is. Fortunately, your vet does know it and will provide you with the right information.
You may check the situation in your country by clicking on one of the link below:

Transmission
Rabies’s virus affects potentially any warm-blooded animal (birds and mammals). But mammals and especially carnivorous mammals are the main vectors of the disease.
This is because carnivorous mammals bite (birds can't bite since they have no teeth). As the virus is transmitted through saliva to blood, it easily enters the body through an open wound caused by a bite.
The virus can’t break into the body through an intact skin.
99% of human cases of rabies are caused by domestic dogs according to the World Health Organization (Rabies vaccines: WHO position paper). But bites by bats are a growing concern since infected bats seem to spread rapidly and their very small bites often remain unnoticed.
However, the main reservoir of rabies viruses are wild animals: foxes, coyotes, ferrets, bats, groundhogs…They may infect domestic dogs or cats which then become infecting vectors of the virus.
No need to say that transmission from human to human is very rare.
Mechanisms of progression
After a bite of an infected animal, the virus starts replicating at the wound site. More often it is in muscular tissues. This local replication phase is long; it lasts for 1 to 3 months.
Then the virus reaches peripheral nerves that innervate the infected muscle. It keeps on replicating while moving upward, toward the dorsal root ganglia, the spinal cord and the brain. The progression continuously accelerates. The closer to the brain, the quicker.
By moving along the nerves, instead of circulating in the blood or the lymph, it escapes from the defenses of the immune system.
Once rabies virus has reached the brain, it causes there an inflammation (encephalitis). At the same time, it disseminates to other organs in the body along the nerves.
Because they are close to the brain, the organs within the head are hit first. Especially, the salivary glands are rapidly enabled to spread infecting viruses in the mouth.
Domestic dogs can shed viruses from their saliva for several days before the first symptoms occur. This means in practice that a dog may become infective before the owner has a chance to notice that something is going wrong.
Symptoms
Due to the long incubation period, the symptoms show up several weeks after the dog has been bitten.
The symptoms are neurological. The behavior of the dog suddenly changes. It produces an excessive amount of saliva it can’t swallow. There are 2 forms of the disease.
Furious form
Dogs infected with rabies become very aggressive and threatening. They show their teeth and seem to ignore any kind of danger. They are prone to biting or scratching at any occasion. They bite or eat objects of any nature, or even feces as if they were looking for a way to overcome the discomfort of their excessive salivation.
Of course, they can bite other animals or people. This is the way the disease is transmitted.
This is the “mad-dog” syndrome. This insanity doesn’t last long, no more than a week. The poor dog then falls into a coma and dies.
Paralytic form
The owner notices a lack of physical coordination and balance. The throat and the masseter muscles get paralyzed. The dog is not aggressive, but its saliva remains contagious and the contact of an open wound allows the transmission of the virus.
Coma and death follow within a short period of time.
Outcomes
Once the symptoms appear, the disease causes the death of the animal within a few days.
Treatment and prevention
As you can understand now, Rabies is quite a serious health issue.
It causes the death of tens of thousands people around the world. The situation is quite unequal though, since 95% of them occur in Asia and Africa. In Western Europe, the disease is almost eradicated.
In North America, there are also very few cases of human rabies. But, eradication doesn’t seem achievable here because of the huge wild animal reservoir.
For their own safety, any dog should be vaccinated against rabies, unless it lives in a very safe environment. The vaccination schedule consists of an initial single dose followed by boosters every 1 to 3 weeks according to local legal requirements.
What to do if a man or a woman is bitten by a dog?
Any domestic dog, even vaccinated, that bites a human should be suspected to be rabid and isolated under quarantine for at least 10 days. If the animal develops the symptoms of rabies, it should be euthanized and submitted to laboratory investigations.
If rabies is confirmed or suspected (in case the animal has not been identified or analyzed), the person who has been bitten should receive a post exposure prophylaxis which consists of:
- Extensive wound washing
- A series of vaccinations as recommended by the WHO
- Rabies immunoglobulin, if necessary
Table: Categories of contact and recommended post-exposure prophylaxis (PEP)
| Categories of contact with suspect rabid animal | Post-exposure prophylaxis measures |
|---|---|
| Category I – touching or feeding animals, licks on intact skin | None |
| Category II – nibbling of uncovered skin, minor scratches or abrasions without bleeding | Immediate vaccination and local treatment of the wound |
| Category III – single or multiple transdermal bites or scratches, licks on broken skin; contamination of mucous membrane with saliva from licks, contacts with bats. | Immediate vaccination and administration of rabies immunoglobulin; local treatment of the wound |
Source: World Health Organization
Some US states recommend sticking with the Compendium of Animal Rabies Prevention and Control
Main references
Canine Distemper Virus (CDV)
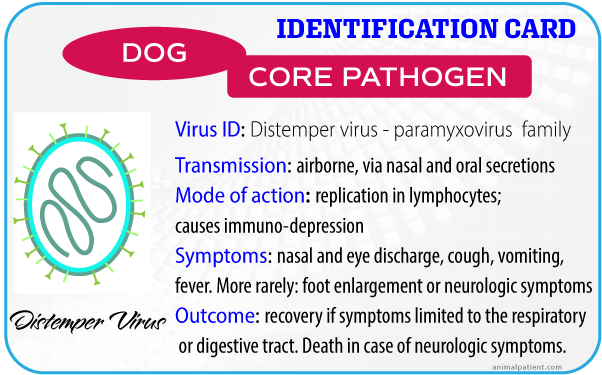
Canine distemper virus is a paramyxovirus. It is related to the human’s virus that causes measles.
Transmission
Your dog can catch the virus from another animal’s nasal and pulmonary secretions. Contamination is usually airborne. Small droplets containing the virus find their way to the mouth, the nose or the pulmonary mucosa.
Infection by eating contaminated meat is still possible, but less frequent.
An infected animal is contagious for several months.
Canine distemper virus can contaminate wild carnivorous animals such as foxes, coyotes, wolves, minks, otters, weasels, skunks, martens, fishers, wolverines or raccoons. They are a reservoir for the virus. As a consequence, it’s impossible to eradicate CDV by vaccinating only domestic animals.
The exposure of your dog to other dogs or to wild animals increases the risk that it gets infected.
Mechanisms of progression
As for any other virus, canine distemper viruses need a host cell to replicate. Ironically, CDVs replicate in the cells of the primary immune system: macrophages and monocytes located in the lymphatic tissues of the respiratory tract, the cells that are precisely supposed to destroy viruses.
The infection weakens the immune system (= immunosuppression), and the first consequence is an increased susceptibility to bacterial infections.
Then the virus reaches the lymph nodes, the spleen, the thymus, the bone marrow and various mucosal tissues in the digestive tract or in the eyes.
At this stage, if the dog’s immune system isn’t strong enough to react, the infection leads to serious complications, especially on the central nervous system, and often to death.
Symptoms
Canine distemper virus induces a wide range of symptoms. They are not specific to the disease. It makes the diagnosis difficult.
The disease is progressive. It starts by a short period of mild fever and anorexia.
A few days later, the fever worsens, and you will notice your dog shows nasal and eye discharge, it will cough and may vomit if the virus reaches the digestive tract.
Sometimes the dog’s feet enlarge up to three times: this is the hard pad disease.
Depending on the strength of the dog’s immune system, the virus may finally attack the nervous system. In this case, the infected dog develops neurologic symptoms such as a lack of muscle coordination, compulsive movements, intense salivation and paralysis.
Treatment
The first precaution is to keep the infected dog away from other dogs so that it can't contaminate them.
As there is no available anti-viral drug that has an effect against canine distemper virus, the treatment is only supportive. It consists of treating the symptoms or the consequences of the infection:
- anti-infectives against secondary bacterial infection
- fluid therapy in case of digestive disorders (diarrhea, vomiting)
- attempts to control neurologic disorders
Prognosis
If the dog receive rapid and intensive care, and if the symptoms are limited to the respiratory and digestive tracts, it may well recover.
In case of neurological disorders, the prognosis is guarded and the outcome is often the death of the animal.
Prevention
The only effective preventive measure is vaccination.
You may well also try to keep your dog away from contaminating sources: other dogs or wild animals, especially if it is a young puppy.
Vaccination schedule
The vaccination protocols for adenovirus, parvovirus and distemper virus are identical.
A puppy needs to get vaccinated three times. The first administration takes place at 4-6 weeks of age, and then 2 to 4 weeks later for the second and again.
Another vaccination is strongly recommended for dogs at 6 months OR at 1 year, and then every three years (4, 7, 11 ...).
Main references
Canine Adenovirus
There are 2 types of canine adenovirus (CAV): the type 1 and the type 2. They cause quite different diseases.
But they are closely related and share a lot of common antigens. Vaccines containing live attenuated viruses of CAV type 2 immunize for both CAV type 2 and type 1.
Canine adenovirus type 1 causes Infectious Canine Hepatitis also known as Rubarth disease. It attacks the kidney, the liver and blood vessels.

Canine adenovirus type 2 is one of the main causes of the most severe forms of kennel cough.

Besides, it's worth noting that adenoviruses are nowadays a popular subject in human medicine research. They can be used as viral vectors for gene therapy in some major areas such as cancer, innovative vaccines or neurodegenerative diseases.
Transmission
Adenoviruses are very contagious. They are primarily transmitted by the urine, the feces or the saliva. They may also be spread through the air.
CAV type 2 can be found in other carnivorous mammals such as foxes or coyotes.
This virus is very contagious. Dogs keep on shedding viruses via the urine for months after healing. To prevent the spread of the infection, any infected animal should be kept isolated from other dogs for many days.
Adenoviruses are very resistant in the outside environment where they can survive for several days. Dogs and puppies often get infected by viruses surviving in the environment, without any direct contact with an infected animal.
Mechanisms of disease progression
CAV type 1 is the virus responsible for Rubarth’s disease (i.e. Infectious Canine Hepatitis). The virus first settles in the mouth, tonsils and throat where it replicates for a period of 4 to 7 days.
Then it migrates to other places in the body: the liver tissue or the blood vessels. It may also colonize the eyes, the kidneys, the spleen and the lungs.
It attacks the walls of blood vessels and affects the clotting ability of blood. Thus, the main consequences of the infection are bleeding and hemorrhage.
In the liver, it causes the destruction of hepatocytes (liver cells). In the kidneys it induces glomerular lesions (see glomerulus).
CAV type 2 is one of the causes of tracheobronchitis, the other name for Kennel Cough. Other viruses (parainfluenza, influenza...) or bacteria (Bordetella, Mycoplasma) may also cause tracheobronchitis.
The disease occurs more frequently when dogs are grouped in the same place (shelters, rescue centers, breeding kennels, or pet stores) hence the name “Kennel Cough”.
After an incubation period of 3 to 10 days the virus colonizes the trachea and the upper respiratory tract. It induces lesions in the epithelium of bronchi and an inflammation of the tonsil and the pharynx.
Symptoms
Adenovirus type 1
Symptoms range from very mild to hyperacute.
Adenoviruses cause fever.
In the milder cases, the fever doesn’t last more than one day. In more severe cases, the fever persists and other symptoms develop. They include apathy, lack of appetite, excessive drinking, eye inflammation, discharge from the eyes and nose, and sometimes belly pain and vomiting.
The increase in blood clotting time induces hemorrhages in many organs. It may cause the gum to bleed. In the most severe forms of the disease, the central nervous system is affected. It results in convulsions and/or paresis (loss of voluntary movements). You may also, but rarely, notice a lack of coordination in the dog’s movements or even blindness.
The dog may also be affected with the "blue-eye" symptoms. It comes from the replication of the virus in the corneal endothelium. This episode takes place a few days after the beginning of the infection. This symptom may also occur after administration of an adenovirus vaccine. It doesn't last long.
Adenovirus type 2
The most characteristic symptom is a dry cough that sounds almost as a goose honk.
Other signs include runny nasal discharge and inflammation of the tonsil and pharynx.
Also, as for many other viruses, adenoviruses open doors to bacterial superinfections that worsen the symptoms.
Outcomes
Adenovirus type 1
In the most serious cases, especially in puppies, adenoviruses type 1 cause death and sometimes very rapidly.
In most cases, dogs recover slowly. But they may develop a liver or a kidney chronic disease afterward.
Sometimes the corneal disorder can't be cured and progresses into glaucoma.
Adenovirus type 2
Of the two adenoviruses, CAV-2 is the less harmful. Most often, the disease is mild and ends within a few weeks.
There are some exceptions though. In weaker individuals, puppies or aging dogs, a secondary pneumonia may develop and possibly lead to the death of the dog.
Treatment and prevention
Treatment
No treatment is available against adenoviruses. Your vet can only take care of symptoms. It will increase the chances your dog’s immune system gets rid of the infection.
Depending on the symptoms, the supportive care may include:
- anti-inflammatories
- anti-infectives (against a possible bacterial superinfection)
- a custom diet plan
- treatments for the liver or the kidneys.
- treatments for the control of diarrhea, vomiting or hemorrhages
- some rest: the dog should be kept quiet and calm
Prevention
CAV-2 vaccines have less adverse effects than CAV-1 vaccines and offer cross protection against both viruses.
This is why available commercial vaccines are made of live attenuated strains of canine adenoviruses type 2. They will protect your dog against both CAV type 1 and type 2.
Vaccination schedule
It is the same as for parvovirus and distemper virus:
Puppies get vaccinated three times, at 4-6 weeks of age, and then every 2 to 4 weeks.
Adult dogs are vaccinated at 6 months OR at 1 year, and then every three years (4, 7, 11 ...).
Main references
Canine Parvovirus type 2 (CPV-2)
Parvoviruses type 2 attack mainly the digestive tract. They cause diarrhea and vomiting. In puppies, they cause very severe symptoms that often lead to death.

Transmission
Canine parvovirus is a very contagious virus.
It can be found in dogs, coyotes, wolves, foxes. Some strains (CPV 2a and 2b) can also infect cats. All these species are reservoirs for the virus.
Canine parvovirus is shed in very large quantities in the feces of infected animals. It is very resistant in the outside environment, and can survive from several weeks to a few years under favorable conditions.
It can be carried under a dog’s foot or hair and disseminated that way. There are more risks of contamination in places usually visited by dogs such as pet stores, breeding kennels or animal shelters.
Canine parvoviruses enter the body through oral contact. The dog or puppy gets the infection by licking itself, or a contaminated ground.
An infected dog usually starts shedding viruses in its feces after an incubation period of only 4 days, and keeps on shedding for weeks well after the symptoms have disappeared. This adds to the contagiousness of the disease.
Mechanisms of progression
After entering the body through the dog’s mouth, the virus first colonizes the mouth’s and pharynx’s tissues and the lymph nodes where it starts replicating.
After 3 to 4 days, it then migrates to various organs. But, it is to the digestive tract that the virus does the most damage.
Intestines are covered with small villi that look like tiny hair. In reality they are thin and long protuberances of the intestinal wall and play a very important role in the absorption of nutriments. Canine parvovirus 2 use villi cells to replicate in numbers and eventually destroy them.
Another notable target of the virus is the heart. It causes heart enlargement, especially on its left side.
Symptoms
The symptoms evolution is rapid. Vomiting episodes precede diarrhea, anorexia and dehydration that requires emergency care.
Bacterial superinfection may accelerate and worsen the symptoms.
The virus may also cause acute or chronic cardiac failure.
Outcomes
Unvaccinated puppies are very sensitive to the virus. They often die from being infected.
The puppies that survive for the first 4 days of the enteric form of the disease usually recover after one week. But still, few of them may develop a secondary and fatal heart disease.
Adult dogs are more resistant, but some can still die from the infection.
Some dog breeds are reported to be more sensitive to the virus: Alaskan sled dogs, American Staffordshire terriers, American Pit Bull terriers, Doberman pinschers, English Springer spaniels, German shepherds, Labrador retrievers, and Rottweilers.
The good news is that the dogs that survive the infection are immunized.
Treatment and prevention
The treatment consists of controlling the consequences and possible complications of the infection. Basically, infected dogs receive a fluid therapy against dehydration and anti-infectives against a possible bacterial superinfection.
Prevention starts by vaccinating puppies according to the recommendations.
Every dog that are or supposed to be infected by the virus should be prevented from disseminating the pathogen. A strict isolation procedure from other animals is recommended. The floors should be cleaned with a bleach-based solution.
Vaccination schedule
It is the same as for adenovirus and distemper virus:
Puppies get vaccinated three times, the first at 4-6 weeks of age, and then every 2 to 4 weeks.
Adult dogs are vaccinated at 6 months OR at 1 year, and then every three years (4, 7, 11 ...).

